Welcome to the land of radiotherapy: Witness the waiting room filled with glossy magazines; revel at the sight of chocolate bars on sale behind the counter; marvel at the doors, whose signage warns of radiation; tremble at the nurses calling you in for consultation. And get your parking validated, too.
 Yesterday Zsolt and I went in for a planning session. It was really quite simple, and surprisingly we didn’t wait in the waiting room for an hour. They called me in before I could settle with a magazine.
Yesterday Zsolt and I went in for a planning session. It was really quite simple, and surprisingly we didn’t wait in the waiting room for an hour. They called me in before I could settle with a magazine.
“Catherine Brunelle?”
“Here!”
And in we went. I was taken into the CT scanning room, and the nurse explained the process.
“I’m Karen, and that’s Louise, and Shelley, and Amy, and Tanya.”
“Hi! Hi. Hello! Hey.” (a chorus of hellos from the nurses – all so very friendly)
“We’ll be scanning you today and making marks on your body.”
Apparently I was to have a CT scan, but no injections or dyes were needed (thank goodness, my last CT scan I had to drink a litre of Koolaid dye in about thirty minutes. Ugh). The doctor would come in and put marks on my chest (around the scar/breast area), they would then line me up, draw more lines, take the scan and give me some tattoos.
Here is how you are measured: They have you put your butt against this cushion and lay back into a head rest. The table is a table, no cushioning. Feet are placed against some plastic slider that keeps them steady. Arms are raised together over the body, then back above the head into some arm rests. There’s some strange medical bondage happening behind hospital doors, but all in the name of health management. It reminded me of old torchure devices, except everyone was smiling and happy, and I wasn’t uncomfortable, and there wasn’t any pain. So maybe a torture device isn’t the best description . . .
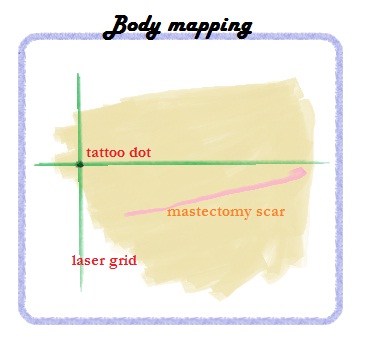
The doctor came in and wrote with green marker around my right chest area. All the while I stared at the ceiling. Finally it was time for the CT scan. This scan is designed to map out the dips and bumps of my chest wall, as well as measure where each type of tissue starts/ends (e.g. lung, rib, skin, etc.). Therefore, when I get my radiotherapy, the machine will account for those differences and change so that my lung gets less radiation than my skin. It’s a good thing.
The nurses taped little wires and buttons to my chest according to the doctor’s instructions. Afterwards the nurses and doctors left the room and the machine began to whirr. Slowly I was slid back and forth through a giant grey doughnut (CT machine) and something in that doughnut spun around me – this, I later was told, was taking x-rays in a spiral motion. The CT scan lasted about five minutes.
Finally it was time for the tattoos! Ugh! Three permanent tattoos are required for radiotherapy: one in the middle of my chest, and two on either side of my body. They line you up on a laser grid and mark the places.
Here is how they administer the tattoo: a drop of ink is placed on the body. The nurse then makes a semi-deep prick of her needle into your skin, through the ink. That’s all. I guess the ink seeps in behind the needle and stays. I now have three tiny, dark dots across my body. They are too small to resemble moles, maybe small blackheads is a better description. Clogged pores.
It could have been worse.
And after all this, the nurses gave me my schedule for radiotherapy. Guess what? I don’t start for THREE WEEKS! How bizarre. I feel as though someone has extended my vacation.
Finally, cherry on the top of my day, I took my fist tamoxifen pill yesterday. This drug is designed to scoop up estrogen before cancer can take advantage, and it’s intended to be taken for five years. We’ll see.
One step at a time – and look no further. For the time being I have three weeks off, which sounds pretty freaking sweet to me.
And that, in a nutshell, was the radiotherapy planning session.



